Boot Camp 2022: A Short Course on Genetics and Genomics
Unfortunately, Boot Camp 2020-2021 has been cancelled due to COVID-19. We hope to offer the next Boot Camp in summer 2022!
For our online learning opportunity, please see Basic Training, A Course in Reproductive Medical Genetics
Overview
 We have assembled an outstanding faculty of leading experts for this one week, interactive and intensive short course in genetics and genomics as it relates to reproductive medicine. The course will provide a comprehensive overview of inheritance, genetic disease, cyto-, molecular and clinical genetics, and the most up-to-date information on the latest in next generation sequencing and genetic testing. The program includes lectures, symposia, workshops, laboratory demonstrations, case reviews, panels, and a number of distinguished speakers. We have a large and diverse faculty and a curriculum that will allow substantial faculty-student interaction. With only 30 attendees, we are able to conduct hands on workshops and discussions exploring genomic technologies and case-based learning. Molecular technologies will be emphasized.
We have assembled an outstanding faculty of leading experts for this one week, interactive and intensive short course in genetics and genomics as it relates to reproductive medicine. The course will provide a comprehensive overview of inheritance, genetic disease, cyto-, molecular and clinical genetics, and the most up-to-date information on the latest in next generation sequencing and genetic testing. The program includes lectures, symposia, workshops, laboratory demonstrations, case reviews, panels, and a number of distinguished speakers. We have a large and diverse faculty and a curriculum that will allow substantial faculty-student interaction. With only 30 attendees, we are able to conduct hands on workshops and discussions exploring genomic technologies and case-based learning. Molecular technologies will be emphasized.
Boot Camp is limited to 30 clinical fellows or physicians in their first two years of an academic faculty appointment who are recommended by their chair or fellowship director. The program is geared to maternal fetal medicine, reproductive endocrinology, gynecologic oncology and general obstetrics and gynecology physicians. Through unrestricted educational grants, we have created an opportunity for tuition free education that includes support for lodging and some meals. The University of California San Francisco has generously agreed to host the second offering of this annual course.
Applications
Applications will be available here January 2022
Thirty applicants will be selected
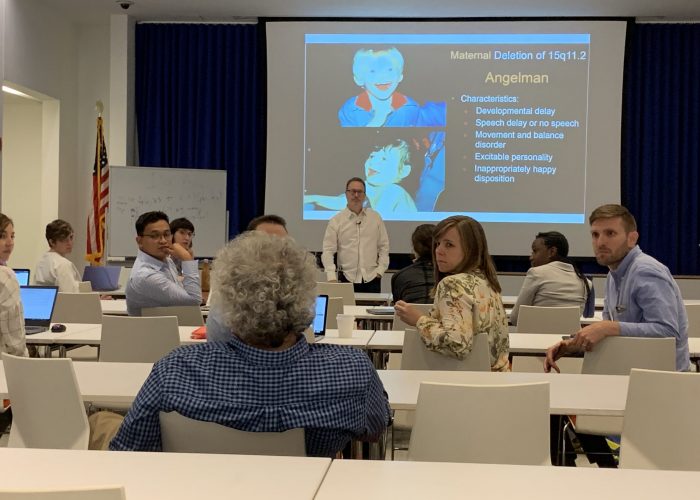
Photo Gallery
Curriculum
- The Genome, Gene Structure and Function
- Mechanisms and Modes of Inheritance
- Cytogenetics and Microarray
- Molecular Technologies
- Exome and Genome Analysis
- Variant Classification
- Prenatal and Pediatric Dysmorphology
- Genetics of Pregnancy Loss and Infertility
- Preimplantation Genetic Testing
- Mosaicism in Reproductive Medicine
- Quandaries in Embryo Selection
- Genetic Counseling to Support Patient Decision Making
- Case Studies in Expanded Carrier Screening
- Case Studies in Noninvasive Prenatal Testing
- Maternal Genetic Disease
- Newborn Screening and Expanded Carrier Screening
- Genetic Evaluation of Fetal Anomalies
- Case Studies in Fetal Anomaly Evaluation
- The Prenatal Exome
- Genetic Basis of Cancer
- Cancer Genetics in Women’s Health
- Polygenic Risk and Genetics of Complex Disease
- Genetic Screening Across the Life Span
Daily Schedule
8:15
Daily Announcement
8:30-9:15
Lecture
9:15-10:00
Lecture
10:00–10:30
Break
10:30-11:15
Lecture
11:15-12:00
Lecture
12:00-1:00
Lunch with Faculty
1:00-2:15
Workshop 1
2:30-3:45
Workshop 2
4:00-5:15
Lecture
Course Directors
 |
Mary E. Norton MDUC San FranciscoDr. Mary Norton is a perinatologist and geneticist, and is a Professor in the Department of Obstetrics, Gynecology and Reproductive Sciences at UCSF. She is Director of the Division of Maternal-Fetal Medicine and co-Director of the UCSF Center for Maternal-Fetal Precision Medicine. Her clinical and research interests include genetic testing and its application to prenatal screening and diagnosis. She focuses on the unique aspects of translating new genetic and genomic technologies into improved care for pregnant women and their fetuses. Much of her research has involved cell free DNA screening and implementation into practice, as well as patient and provider education regarding prenatal genetics’ generally, and cfDNA specifically. |
 |
Ronald Wapner MDColumbia UniversityDr. Wapner is the Director of Reproductive Genetics and the Vice Chair of Research in Obstetrics and Gynecology for Columbia University Irving Medical Center. Dr. Wapner is an internationally known physician and researcher specializing in reproductive genetics. He pioneered the development of chorionic villus sampling (CVS) and multi-fetal reduction. He has authored or co-authored over 400 publications and he has been an active investigator in the area of Maternal-Fetal Medicine and recently led a multicenter study evaluating the accuracy, efficacy, and clinical advantages of prenatal diagnosis using microarray analysis. He has had a significant role in the development of multidisciplinary research studies and clinical research centers throughout his career. |
Course Facilitator
 |
Janice G. Edwards, MS, CGCUniversity of South CarolinaJanice G. Edwards, MS, CGC serves as Director of the University of South Carolina School of Medicine Genetic Counseling Program and has over 35 years in clinical practice focused on prenatal genetics and more recently, Huntington disease. An experienced genetic counselor educator, she is also Founding President of the Transnational Alliance for Genetic Counseling, an international network of genetic counselor educators.. She has directed genetic education conferences and symposia regionally, nationally and internationally. A skilled facilitator, Ms. Edwards has also worked with several national organizations to build consensus around emerging issues in reproductive genetics. She is committed to supporting clinicians and healthcare systems in the integration of genetics and genomics in medicine. |
Faculty
 |
Vimla Aggarwal, MDColumbia UniversityDr. Vimla Aggarwal is an American Board of Medical Genetics and Genomics (ABMGG) certified Clinical Molecular Geneticist and Cytogeneticist. She directs the Precision Genomics Laboratory, a CLIA- certified laboratory at Columbia University Irving Medical Center. She has been deeply involved in the transition of genomic technologies (like chromosome microarrays, genotyping arrays, next generation sequencing panels as well as whole exome sequencing) from a research space to a clinical setting. Her research interests lie in the elucidation of the molecular basis for undiagnosed genetic diseases, as well as methods to improve variant classification and interpretation. |
 |
Wendy Chung, MD, PhDColumbia UniversityWendy Chung, M.D., Ph.D. is a clinical and molecular geneticist andthe Kennedy Family Professor of Pediatrics and Medicine. She received her B.A. in biochemistry and economics from Cornell University, her M.D. from Cornell University Medical College, and her Ph.D. from The Rockefeller University in genetics. Dr. Chung directs NIH funded research programs in human genetics of obesity, breast cancer, pulmonary hypertension, autism, and birth defects including congenital diaphragmatic hernia and congenital heart disease. She leads the Precision Medicine Resource in the Irving Institute At Columbia University. She has authored over 350 peer reviewed papers and 50 reviews and chapters in medical texts. She was the recipient of the American Academy of Pediatrics Young Investigator Award, the Medical Achievement Award from Bonei Olam, a career development award from Doris Dukeand the NY Academy of Medicine Medal for Distinguished Contributions in Biomedical Science. Dr. Chung is renowned for her teaching and mentoringand received Columbia University’s highest teaching award, the Presidential Award for Outstanding Teaching. She was the original plaintiff in the Supreme Court case that overturned the ability to patent genesand served on the Institute of Medicine Committee on Genetic Testing. Dr. Chung enjoys the challenges of genetics as a rapidly changing field of medicine and strives to facilitate the integration of genetic medicine into all areas of health care in a medically, scientifically, and ethically sound, accessible, and cost effective manner. |
 |
Patrick Devine, MD, PhDUC San FranciscoPatrick Devine, M.D., Ph.D., is an Assistant Professor in the Department of Pathology at the University of California, San Francisco School of Medicine. He is an anatomic pathologist with additional fellowship training and expertise in molecular and genetic pathology. He serves as an attending pathologist at the Clinical Cancer Genomics Laboratory (CCGL) at UCSF as well as the Genomic Medicine Laboratory at UCSF. He obtained his medical and graduate degrees at Stanford Medical School and has been involved in several basic research projects characterizing the genetic and cellular origins of cardiac malformations. |
 |
Katherine M. Hyland, PhDUC San FranciscoDr. Katherine M. Hyland is a Professor in the Department of Biochemistry and Biophysics and the Institute for Human Genetics at the UCSF School of Medicine. Her primary roles are in health professions education and faculty development. Dr. Hyland received a BS in Biochemistry from Virginia Tech, an MS in Molecular Cytogenetics from Rutgers University, and a PhD in Human and Molecular Genetics from Johns Hopkins University. She completed postdoctoral training at the University of British Columbia, Centre for Molecular Medicine and Therapeutics, and the UCSF Comprehensive Cancer Center. In her current position, she teaches genetics, molecular biology and biochemistry, emphasizing clinical applications of foundational sciences using innovative educational modalities. She directs the medical genetics and genomics curriculum in the School of Medicine, and Chairs the Medical Genetics Curriculum Committee and the Institute for Human Genetics Education Committee. She has been actively involved in designing and implementing the UCSF Bridges medical curriculum. Dr. Hyland is active member in the Haile T. Debas Academy of Medical Educators and leads Faculty Development workshops both at UCSF and as well as nationally and internationally. She served as the inaugural Chair of the Medical Genetics Course Directors group in the Association of Professors of Human and Medical Genetics (APHMG), led an effort to develop national competencies in medical genetics, and currently serves as Secretary/Treasurer in the APHMG Leadership Council. She is also an active a member of the International Association of Medical Science Educators (IAMSE), the American Society of Human Genetics (ASHG), the Association of Biochemistry Educators (ABE), the Western Group on Educational Affairs (WGEA), and the Inter-Society Coordinating Committee for Practitioner Education in Genomics (ISCC). Her current educational interests include encouraging students to engage in curiosity and the process of discovery, applying the concept of cognitive integration, and incorporating an integrated approach to genomic medicine in the training of future and current physicians. |
 |
Barbara A. Koenig, PhDUC San FranciscoBarbara A. Koenig, Ph.D., is Professor of Bioethics and Medical Anthropology, based at the Institute for Health & Aging, University of California, San Francisco. She is the Director of the UCSF Program in Bioethics, a program that spans ethics research, clinical ethics, and ethics education across the university’s four professional schools. Prof. Koenig pioneered the use of empirical methods in the study of ethical questions in science, medicine, and health. Prof. Koenig’s current focus is emerging genomic technologies, including biobanking policy and using deliberative democracy to engage communities about research governance. Her work has been continuously funded by the National Institutes of Health since 1991. Currently, she: 1) directs the ELSI component of a Chan Zuckerberg Biohub award focused on interpretation of rare variants in newborn screening, 2) is P.I. of UCSF’s Program in Prenatal and Pediatric Genomic Sequencing (P3EGS), part of the CSER2 national network, and, 3) is supported by NCI to conduct an “embedded ethics” study of the Athena “Wisdom” PCORI-funded clinical trial of genomic risk-stratified breast cancer prevention. Previously, she directed an NHGRI-funded “Center of Excellence” in ELSI Research. Prof. Koenig was the founding executive director of the Center for Biomedical Ethics at Stanford University; she created and led the Bioethics Research Program at the Mayo Clinic in Rochester, Minn. She received her Ph.D. from the University of California, Berkeley and San Francisco joint program in Medical Anthropology. Prof. Koenig is an active participant in policy, having served on the ethics committee that advises the director of the CDC and the Department of Health and Human Services “Secretary’s Advisory Committee on Genetic Testing.” She recently served on a state-wide “Health Data Governance Task Force” which advised the University of California’s president. Her most recent book is “Revisiting Race in a Genomic Age.” |
 |
Brynn Levy, MSc (Med), PhDColumbia UniversityBrynn Levy, M.Sc. (Med), Ph.D. is a Professor of Pathology and Cell Biology at the Columbia University Medical Center. He is also the Director of the Clinical Cytogenetics Laboratory of the New York Presbyterian Hospital and a Co-Director of the Division of Personalized Genomic in the Department of Pathology & Cell Biology. Dr. Levy is regarded internationally as an expert in the clinical utility of genomic technologies in reproductive medicine. He has authored multiple book chapters and publications on molecular genetics, clinical cytogenetics and molecular cytogenetics and lectured internationally about his experience utilizing CGH and high resolution SNP microarrays both as a clinical and research tool. His research areas of interest include early prenatal screening using fetal cells and cell-free fetal DNA from maternal circulation, PGD and the etiology of recurrent miscarriage. Dr. Levy was a Co-Investigator of the Multicenter NICHD study that investigated the use of microarrays for prenatal diagnosis and was the Columbia University site Principal Investigator of a NIH-funded study from the Stillbirth Collaborative Research Network (SCRN) that assessed CNVs in stillbirths. Dr. Levy is the past President of the Cancer Genomics Consortium (GCC) and was the PI at Columbia University Medical Center for the GCG Multi-center Quality Control trial that performed cross-platform validation of cytogenomic arrays for cancer diagnostics. Dr. Levy currently serves as the Genetics and Genomics Section Editor for the journal Prenatal Diagnosis. |
 |
Billie Lianoglou, LCGC MSUC San FranciscoBillie Lianoglou is a genetic counselor who specializes in prenatal care. She works closely with perinatologists to educate families on potential genetic risks for fetal abnormalities or complications. Billie splits her time between working with families at the UCSF Fetal Treatment Center and supporting the research of genetic specialists Dr. Mary Norton and Dr. Teresa Sparks at the UCSF Center for Maternal-Fetal Precision Medicine. This research explores the value of prenatal whole exome sequencing in the setting of fetal anomalies and complications including non-immune hydrops fetalis. |
 |
Bryce Mendelsohn, MD, PhDKaiser Permanente Oakland Medical CenterDr. Bryce Mendelsohn went to medical school at Washington University in St. Louis where he earned his MD and a PhD in Molecular Genetics and Genomics. He completed residencies in Pediatrics and Medical Genetics at UCSF, as well as a postdoctoral fellowship at the Gladstone Institute of Neurology Disease studying mitochondrial metabolism. He was on the faculty at UCSF for two years , where he split his time between metabolic genetics and spearheading several precision medicine programs, before moving to Kaiser Permanente Oakland Medical Center. His interests include rare disease diagnosis, metabolic and mitochondrial disease, newborn screening, and precision health. |
 |
Tippi MacKenzie, MDUC San FranciscoTippi MacKenzie is a pediatric and fetal surgeon who is focused on developing better ways to diagnose and treat genetic diseases before birth. She runs a translational research lab examining fetal immunology and maternal-fetal tolerance, with the ultimate goal of inventing new fetal therapies for patients with genetic diseases or pregnancy complications. She is the Principal Investigator on the world’s first Phase 1 clinical trial to perform in utero hematopoietic stem cell transplantation to treat fetuses with alpha thalassemia. Her research has been supported by the National Institutes of Health, the March of Dimes, the California Institute for Regeneration Medicine, and the Burroughs-Wellcome Fund. Tippi has been awarded the Jacobson Award by the American College of Surgeons for her innovative work.Tippi trained in classical piano at Juilliard before obtaining her undergraduate degree from Harvard College and her medical degree from Stanford University. She completed her surgical residency at Brigham and Women’s Hospital in Boston and obtained additional fellowships in Fetal Surgery and Pediatric Surgery at the Children’s Hospital of Philadelphia. She joined the faculty at the University of California, San Francisco in 2007 and is now a Professor of Surgery. In addition to her clinical practice, she is also a member of the Eli and Edythe Broad Institute for Regeneration Medicine and the Biomedical Sciences Program. She recently co-founded the Center for Maternal-Fetal Precision Medicine, with the aim of accelerating the processes that link basic research to clinical trials to improve maternal, fetal, and neonatal health. This Center is testing methods to improve prenatal diagnosis of birth defects and developing new cellular and molecular therapies for definitive fetal treatment. |
 |
Martha Noel, MDUC San FranciscoDr. Martha Noel is a reproductive endocrinologist and infertility specialist, and is an Assistant Professor in the Department of Obstetrics, Gynecology and Reproductive Sciences at UCSF. She attended medical school at Weill Cornell Medical College, completed her OB/GYN residency at New York Presbyterian Hospital – Cornell, and her REI fellowship at UCSF. Dr. Noel’s primary role is as a clinician, treating patients with infertility. Her areas of research include in vitro fertilization outcomes, and she is a co-primary investigator for the Cytokines, Lipids and Reproduction (CLEAR) Study looking at the role of cytokines and lipids in IVF outcomes of women with endometriosis and PCOS. She is also interested in advocating for increased access to fertility care through mandated insurance coverage, and in improving patient satisfaction with the ART care received. |
 |
Robert L. Nussbaum, MDChief Medical Officer of InvitaeRobert L. Nussbaum, MD is the Chief Medical Officer of Invitae, one of the largest genetic information and diagnostic companies in the world. He is board certified in internal medicine, clinical genetics and clinical molecular genetics, and is a Fellow of the American College of Physicians and the American College of Medical Genetics and Genomics. From 2006-2015, he was the Holly Smith Professor of Medicine at UCSF, Chief of the Division of Genomic Medicine and Medical Director of both the Cancer Risk Program and the UCSF Program in Cardiovascular Genetics. He previously served in the Division of Intramural Research of the National Human Genome Research Institute, NIH, and, before NIH, was a Professor of Human Genetics, Pediatrics and Medicine at the University of Pennsylvania and an Associate Investigator of the Howard Hughes Medical Institute. He received an M.D. in 1975 from the Harvard-MIT Joint Program in Health Science and Technology, internal medicine training at Barnes Hospital/Washington University (1975-1978), and genetics training at Baylor College of Medicine (1978-1981). He is the co-author of over 250 peer-reviewed publications in basic and applied human genetics as well as numerous commentaries, editorials, and textbook chapters. He was elected to the National Academy of Medicine (IOM) in 2004 and the American Academy of Arts and Sciences in 2015. Dr. Nussbaum served as a member of the Board of Directors and President of the American Society of Human Genetics, on the Board of Directors of the American Board of Medical Genetics and Genomics, and was a founding fellow and a member of the Board of Directors of the American College of Medical Genetics and Genomics. For his work in identifying alpha-synuclein as a key protein involved in hereditary (and sporadic) Parkinson disease, he was awarded the Klaus Joachim Zülch-Prize for Neurological Research, the Jay Van Andel Award for Outstanding Achievement in Parkinson’s Disease Research, and the Calne Lectureship from Parkinson Canada for his work on hereditary Parkinson disease. He is co-author with Drs. Roderick M. McInnes and Huntington F. Willard of the popular textbook of human genetics, Thompson and Thompson’s Genetics in Medicine. With his two co-authors, he received the 2015 Award for Excellence in Human Genetics Education from the American Society of Human Genetics. He has received numerous other awards for research, service and education from the University of Pennsylvania, the National Institutes of Health, the University of California San Francisco, and the Lowe Syndrome Association. |
 |
Britton D Rink, MDMount Carmel HealthDr. Rink is Director of Medical Genetics in the Mount Carmel Health System, Columbus, Ohio. She is dual board certified in Maternal Fetal Medicine and Genetics and maintains a practice in both subspecialties. Dr. Rink is the Chair of the ACOG Committee on Genetics after serving on the committee for several years and most recently as the Vice Chair. She has particular interest in prenatal diagnosis, advanced fetal imaging, fetal therapy and recurrent pregnancy loss. Dr. Rink has authored several book chapters and publications on genetic testing and screening in pregnancy. She resides in Columbus, Ohio with her husband and four children. |
 |
Julia Silver, MS, LCGCUC San Franciscopreconception patients, she has a particular interest in working with pregnant women who have complex IVF histories or who personally have a diagnosis of a genetic condition. She has broad research interests ranging from investigating the benefits of mindfulness training for genetic counselors to exploring the utility of expanded carrier screening. Julia is passionate about education and serves as a mentor and teacher for genetic counseling, midwifery, and medical students. |
 |
Teresa Sparks, MDUC San FranciscoDr. Sparks is a Maternal-Fetal Medicine specialist as well as a Clinical Geneticist. She attended medical school at the University of California, San Francisco (UCSF); completed residency in Obstetrics & Gynecology at the Brigham & Women’s Hospital / Massachusetts General Hospital combined program; and completed a combined fellowship in Maternal-Fetal Medicine and Clinical Genetics at UCSF. She additionally earned a Masters of Advanced Study in Clinical Research from UCSF. Dr. Sparks cares for women who are either pregnant or considering a pregnancy, who are at higher risk for a variety of maternal and fetal reasons. She sees patients primarily in the Fetal Treatment Center and the Prenatal Diagnosis Center at UCSF. Dr. Sparks is also the PI of the multicenter HyDROPS study (Hydrops: Diagnosing and Redefining Outcomes with Precision Study), which aims to uncover the genetic etiologies leading to non-immune hydrops fetalis through exome sequencing, detailed phenotyping, and more targeted in utero care. |
 |
Melissa Stosic, MS, CGCColumbia UniversityMelissa Stosic, MS, CGC is an independent consultant in the arena of reproductive genetics with nearly 15 years of experience. She has worked in a broad spectrum of roles including counseling patients, implementing and managing several large research trials, lecturing to providers across the globe about non-invasive prenatal testing, leading a medical education team, developing the clinical aspects for industry products, and launching a reproductive genetics service at an academic institution. She has also been an active member of ClinGen’s CaDRe (Consent and Disclosure Recommendations) committee for the past 5 years. |
 |
Arun Wiita, MD, PhDUC San FranciscoArun Wiita, MD, PhD, is a Clinical Pathologist and physician-scientist in the Dept. of Laboratory Medicine at UCSF. In his clinical duties, Dr. Wiita interprets DNA microarrays for diagnosis of copy number variants causative of genetic disease in the prenatal and postnatal settings. He has a particular interest in the integration of emerging knowledge regarding genome architecture and epigenetics in clinical microarray interpretation. In his research lab, supported by a Doris Duke Charitable Foundation Clinical Scientist Development Award, NIH Director’s New Innovator Award, and Damon Runyon Cancer Research Foundation Breakthrough Award, among others, Dr. Wiita focuses on using chemical biology, mass spectrometry, and genome-engineering tools to make diagnostic and therapeutic advances in blood cancers and CNV-related genetic disease. Dr. Wiita graduated from Princeton University with an AB in Chemistry, obtained his MD and PhD at Columbia University with graduate training in single molecule biophysics, and completed residency training in Clinical Pathology at UCSF. |
 |
Ignatia B. Van den Veyver, MDBaylor College of MedicineIgnatia B. Van den Veyver, M.D. is a Professor in the Department of Obstetrics and Gynecology and the Department of Molecular and Human Genetics in Houston, Texas. She is Director of Clinical Prenatal Genetics at Baylor College of Medicine and Texas Children’s Hospital and a faculty member of the Texas Children’s Hospital Fetal Center. Her clinical translational research focuses on exploring novel genetic and genomic methods of prenatal genetic testing and the complexities of their integration into prenatal care with a specific interest in application of prenatal exomes and genomes, counseling for various new technologies. She is also engaged in collaborative research on development and validation of cell-based non-invasive prenatal diagnosis. She oversees a research laboratory located in the Jan and Dan Duncan Neurological Research Institute where she performs translational and basic research on the molecular genetics and epigenetics of human developmental disorders and reproductive genetics and epigenetics. She has published extensively in these various fields and her research is funded by the NIH and private foundations. She is immediate past president of the International Society for Prenatal Diagnosis. |
 |
Jessica Van Ziffle, PhDUC San FranciscoDr. Jessica Van Ziffle is a molecular geneticist, and Assistant Professor in the Department of Pathology at UCSF. She is an active member of the UCSF Institute for Human Genetics. Her clinical and research interests include the development and implementation of clinical molecular genetic testing at the UCSF Clinical Cancer Genomics Lab (CCGL), and Genomic Medicine Lab (GML). Molecular testing techniques include single gene testing, as well as highly multiplexed deep sequencing technologies. The aim of this testing is to identify therapeutic targets, clarify a patient’s diagnosis, or establish a patient’s molecular diagnosis. Of particular interest are the genomics of hematopoietic malignancies, the heritable causes of these malignancies, and the clinical utility of exome sequencing for inherited, or constitutional, diseases. |